Posterior Tibial Tendon Dysfunction
Posterior tibial tendon dysfunction is one of the most common problems of the foot and ankle. It occurs when the posterior tibial tendon becomes inflamed or torn. As a result, the tendon may not be able to provide stability and support for the arch of the foot, resulting in flatfoot.
Most patients can be treated without surgery, using orthotics and braces. If orthotics and braces do not provide relief, surgery can be an effective way to help with the pain. Surgery might be as simple as removing the inflamed tissue or repairing a simple tear. However, more often than not, surgery is very involved, and many patients will notice some limitation in activity after surgery.
AnatomyThe posterior tibial tendon is one of the most important tendons of the leg. A tendon attaches muscles to bones, and the posterior tibial tendon attaches the calf muscle to the bones on the inside of the foot. The main function of the tendon is to hold up the arch and support the foot when walking.
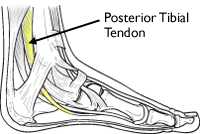 The posterior tibial tendon attaches the calf muscle to the bones on the inside of the foot.
Cause
The posterior tibial tendon attaches the calf muscle to the bones on the inside of the foot.
Cause
An acute injury, such as from a fall, can tear the posterior tibial tendon or cause it to become inflamed. The tendon can also tear due to overuse. For example, people who do high-impact sports, such as basketball, tennis, or soccer, may have tears of the tendon from repetitive use. Once the tendon becomes inflamed or torn, the arch will slowly fall (collapse) over time.
Posterior tibial tendon dysfunction is more common in women and in people older than 40 years of age. Additional risk factors include obesity, diabetes, and hypertension.
Symptoms- Pain along the inside of the foot and ankle, where the tendon lies. This may or may not be associated with swelling in the area.
- Pain that is worse with activity. High-intensity or high-impact activities, such as running, can be very difficult. Some patients can have trouble walking or standing for a long time.
- Pain on the outside of the ankle. When the foot collapses, the heel bone may shift to a new position outwards. This can put pressure on the outside ankle bone. The same type of pain is found in arthritis in the back of the foot.
 The most common location of pain is along the course of the posterior tibial tendon (yellow line), which travels along the back and inside of the foot and ankle.
Doctor Examination
The most common location of pain is along the course of the posterior tibial tendon (yellow line), which travels along the back and inside of the foot and ankle.
Doctor Examination
Medical History and Physical Examination
 This patient has posterior tibial tendon dysfunction with a flatfoot deformity.(Left) The front of her foot points outward. (Right) The "too many toes" sign. Even the big toe can be seen from the back of this patient's foot.
This patient has posterior tibial tendon dysfunction with a flatfoot deformity.(Left) The front of her foot points outward. (Right) The "too many toes" sign. Even the big toe can be seen from the back of this patient's foot.
Your doctor will take a complete medical history and ask about your symptoms. During the foot and ankle examination, your doctor will check whether these signs are present.
- Swelling along the posterior tibial tendon. This swelling is from the lower leg to the inside of the foot and ankle.
- A change in the shape of the foot. The heel may be tilted outward and the arch will have collapsed.
- "Too many toes" sign. When looking at the heel from the back of the patient, usually only the fifth toe and half of the fourth toe are seen. In a flatfoot deformity, more of the little toe can be seen.
 This patient is able to perform a single limb heel rise on the right leg.
This patient is able to perform a single limb heel rise on the right leg.
- "Single limb heel rise" test. Being able to stand on one leg and come up on "tiptoes" requires a healthy posterior tibial tendon. When a patient cannot stand on one leg and raise the heel, it suggests a problem with the posterior tibial tendon.
- Limited flexibility. The doctor may try to move the foot from side to side. The treatment plan for posterior tibial tendon tears varies depending on the flexibility of the foot. If there is no motion or if it is limited, there will need to be a different treatment than with a flexible foot.
- The range of motion of the ankle is affected. Upward motion of the ankle (dorsiflexion) can be limited in flatfoot. The limited motion is tied to tightness of the calf muscles.
Imaging Tests
Other tests which may help your doctor confirm your diagnosis include:
X-rays. These imaging tests provide detailed pictures of dense structures, like bone. They are useful to detect arthritis. If surgery is needed, they help the doctor make measurements to determine what surgery would most helpful.
 (Top) An x-ray of a normal foot. Note that the lines are parallel, indicating a normal arch. (Bottom) In this x-ray the lines diverge, which is consistent with flatfoot deformity.
(Top) An x-ray of a normal foot. Note that the lines are parallel, indicating a normal arch. (Bottom) In this x-ray the lines diverge, which is consistent with flatfoot deformity.
Magnetic resonance imaging (MRI). These studies can create images of soft tissues like the tendons and muscles. An MRI may be ordered if the diagnosis is in doubt.
Computerized tomography scan (CT Scan). These scans are more detailed than x-rays. They create cross-section images of the foot and ankle. Because arthritis of the back of the foot has similar symptoms to posterior tibial tendon dysfunction, a CT scan may be ordered to look for arthritis.
Ultrasound. An ultrasound uses high-frequency sound waves that echo off the body. This creates a picture of the bone and tissue. Sometimes more information is needed to make a diagnosis. An ultrasound can be ordered to show the posterior tibial tendon.
Nonsurgical TreatmentSymptoms will be relieved in most patients with appropriate nonsurgical treatment. Pain may last longer than 3 months even with early treatment. For patients who have had pain for many months, it is not uncommon for the pain to last another 6 months after treatment starts.
Rest
Decreasing or even stopping activities that worsen the pain is the first step. Switching to low-impact exercise is helpful. Biking, elliptical machines, or swimming do not put a large impact load on the foot, and are generally tolerated by most patients.
Ice
Apply cold packs on the most painful area of the posterior tibial tendon for 20 minutes at a time, 3 or 4 times a day to keep down swelling. Do not apply ice directly to the skin. Placing ice over the tendon immediately after completing an exercise helps to decrease the inflammation around the tendon.
Nonsteroidal Anti-inflammatory Medication
Drugs, such as ibuprofen or naproxen, reduce pain and inflammation. Taking such medications about a half of an hour before an exercise activity helps to limit inflammation around the tendon. The thickening of the tendon that is present is degenerated tendon. It will not go away with medication. Talk with your primary care doctor if the medication is used for more than 1 month.
Immobilization
A short leg cast or walking boot may be used for 6 to 8 weeks. This allows the tendon to rest and the swelling to go down. However, a cast causes the other muscles of the leg to atrophy (decrease in strength) and thus is only used if no other conservative treatment works.
Orthotics
Most people can be helped with orthotics and braces. An orthotic is a shoe insert. It is the most common nonsurgical treatment for a flatfoot. An over-the-counter orthotic may be enough for patients with a mild change in the shape of the foot. A custom orthotic is required in patients who have moderate to severe changes in the shape of the foot. The custom orthotic is more costly, but it allows the doctor to better control the position the foot.
Braces
A lace-up ankle brace may help mild to moderate flatfoot. The brace would support the joints of the back of the foot and take tension off of the tendon. A custom-molded leather brace is needed in severe flatfoot that is stiff or arthritic. The brace can help some patients avoid surgery.
Physical Therapy
Physical therapy that strengthens the tendon can help patients with mild to moderate disease of the posterior tibial tendon.
Steroid Injection
Cortisone is a very powerful anti-inflammatory medicine that your doctor may consider injecting around the tendon. A cortisone injection into the posterior tibial tendon is not normally done. It carries a risk of tendon rupture. Discuss this risk with your doctor before getting an injection.
Surgical TreatmentSurgery should only be done if the pain does not get better after 6 months of appropriate treatment. The type of surgery depends on where tendonitis is located and how much the tendon is damaged. Surgical reconstruction can be extremely complex. The following is a list of the more commonly used operations. Additional procedures may also be required.
Gastrocnemius Recession or Lengthening of the Achilles Tendon
This is a surgical lengthening of the calf muscles. It is useful in patients who have limited ability to move the ankle up. This surgery can help prevent flatfoot from returning, but does create some weakness with pushing off and climbing stairs. Complication rates are low but can include nerve damage and weakness. This surgery is typically performed together with other techniques for treating flatfoot.
Tenosynovectomy (Cleaning the Tendon)
This surgery is used when there is very mild disease, the shape of the foot has not changed, and there is pain and swelling over the tendon. The surgeon will clean away and remove the inflamed tissue (synovium) surrounding the tendon. This can be performed alone or in addition to other procedures. The main risk of this surgery is that the tendon may continue to degenerate and the pain may return.
Tendon Transfer
Tendon transfer can be done in flexible flatfoot to recreate the function of the damaged posterior tibial tendon. In this procedure, the diseased posterior tibial tendon is removed and replaced with another tendon from the foot, or, if the disease is not too significant in the posterior tibial tendon, the transferred tendon is attached to the preserved (not removed) posterior tibial tendon.
One of two possible tendons are commonly used to replace the posterior tibial tendon. One tendon helps the big toe point down and the other one helps the little toes move down. After the transfer, the toes will still be able to move and most patients will not notice a change in how they walk.
Although the transferred tendon can substitute for the posterior tibial tendon, the foot still is not normal. Some people may not be able to run or return to competitive sports after surgery. Patients who need tendon transfer surgery are typically not able to participate in many sports activities before surgery because of pain and tendon disease.
Osteotomy (Cutting and Shifting Bones)
An osteotomy can change the shape of a flexible flatfoot to recreate a more "normal" arch shape. One or two bone cuts may be required, typically of the heel bone (calcaneus).
If flatfoot is severe, a bone graft may be needed. The bone graft will lengthen the outside of the foot. Other bones in the middle of the foot also may be involved. They may be cut or fused to help support the arch and prevent the flatfoot from returning. Screws or plates hold the bones in places while they heal.
 X-ray of a foot as viewed from the side in a patient with a more severe deformity. This patient required fusion of the middle of the foot in addition to a tendon transfer and cut in the heel bone.
X-ray of a foot as viewed from the side in a patient with a more severe deformity. This patient required fusion of the middle of the foot in addition to a tendon transfer and cut in the heel bone.
Fusion
Sometimes flatfoot is stiff or there is also arthritis in the back of the foot. In these cases, the foot will not be flexible enough to be treated successfully with bone cuts and tendon transfers. Fusion (arthrodesis) of a joint or joints in the back of the foot is used to realign the foot and make it more "normal" shaped and remove any arthritis. Fusion involves removing any remaining cartilage in the joint. Over time, this lets the body "glue" the joints together so that they become one large bone without a joint, which eliminates joint pain. Screws or plates hold the bones in places while they heal.
 This x-ray shows a very stiff flatfoot deformity. A fusion of the three joints in the back of the foot is required and can successfully recreate the arch and allow restoration of function.
This x-ray shows a very stiff flatfoot deformity. A fusion of the three joints in the back of the foot is required and can successfully recreate the arch and allow restoration of function.
Side-to-side motion is lost after this operation. Patients who typically need this surgery do not have a lot of motion and will see an improvement in the way they walk. The pain they may experience on the outside of the ankle joint will be gone due to permanent realignment of the foot. The up and down motion of the ankle is not greatly affected. With any fusion, the body may fail to "glue" the bones together. This may require another operation.
Complications
The most common complication is that pain is not completely relieved. Nonunion (failure of the body to "glue" the bones together) can be a complication with both osteotomies and fusions. Wound infection is a possible complication, as well.
Surgical Outcome
Most patients have good results from surgery. The main factors that determine surgical outcome are the amount of motion possible before surgery and the severity of the flatfoot. The more severe the problem, the longer the recovery time and the less likely a patient will be able to return to sports. In many patients, it may be 12 months before there is any great improvement in pain.
If you found this article helpful, you may also be interested in Arthritis of the Foot and Ankle.
Source: http://orthoinfo.aaos.org/topic.cfm?topic=A00166
